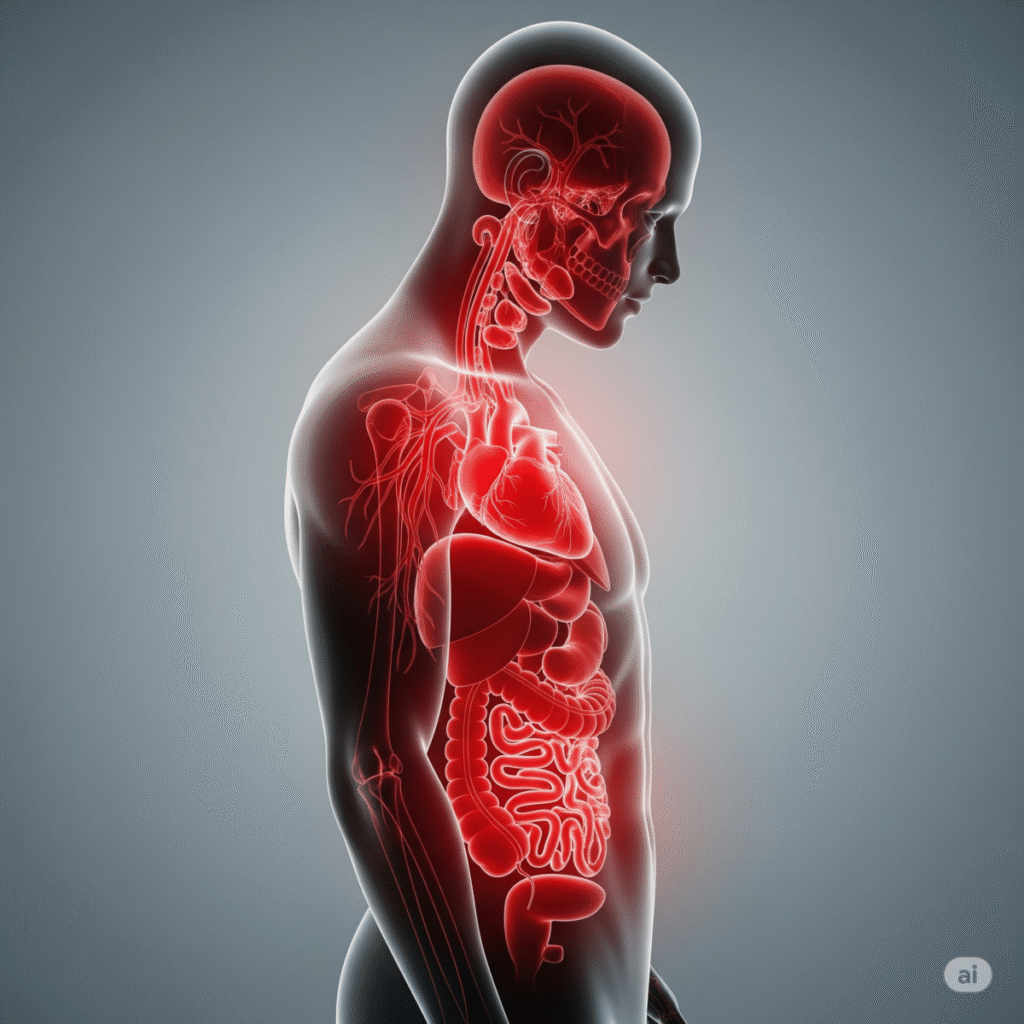
How Stress Transforms Your Body isn’t just a mental health topic—it’s a full-body reality. From digestive issues to heart problems and weakened immunity, chronic stress rewires your internal systems silently. Let’s explore how this happens—and what you can do about it. Sarah’s heart raced as she checked her phone for the third time in five minutes. Work emails flooded in, her teenager needed help with college applications, and her mother’s health was declining. By 3 PM, her shoulders ached, her stomach churned, and she couldn’t remember the last time she slept through the night. Sarah didn’t realize it, but her chronic stress was silently rewiring her body at the cellular level.
If this sounds familiar, you’re not alone. Nearly 77% of Americans regularly experience physical symptoms caused by stress, yet most remain unaware of how stress affects the body on a deeper, more dangerous level. While we often dismiss stress as “just part of life,” emerging research reveals it’s actually one of the most destructive forces acting on our health today—triggering inflammation, weakening immunity, and accelerating aging in ways that can take years off our lives.
The truth is, your body doesn’t distinguish between a charging lion and an overflowing inbox. When stress becomes chronic, it unleashes a cascade of biological changes that can fundamentally alter how your organs function, how your brain processes information, and how your immune system protects you from disease.
What Happens Inside: How Stress Affects the Brain & Hormones
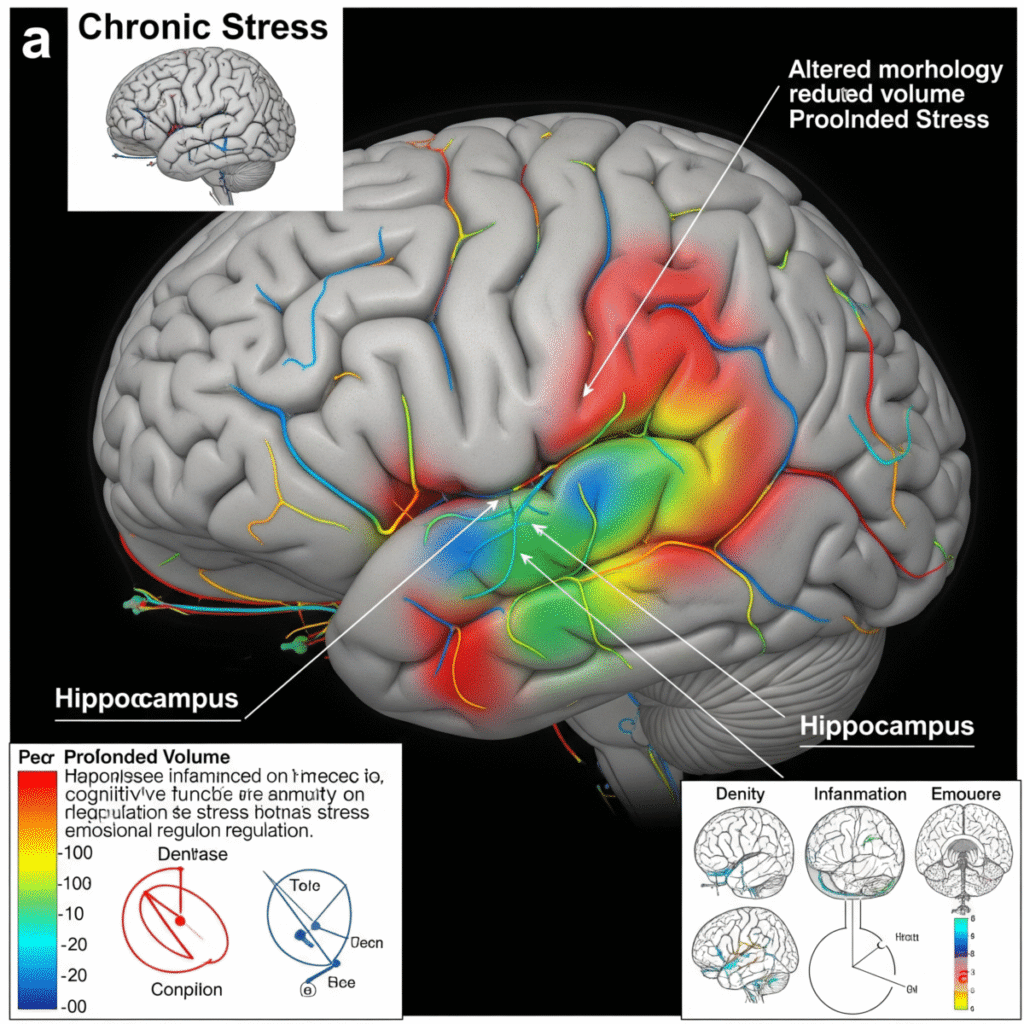
When you encounter stress, your brain’s alarm system—the amygdala—triggers what scientists call the hypothalamic-pituitary-adrenal (HPA) axis. This ancient survival mechanism floods your bloodstream with cortisol and adrenaline within seconds, preparing your body for fight or flight.
In prehistoric times, this response lasted minutes. Today, it can persist for months or years.
Dr. Robert Sapolsky, a Stanford neuroendocrinologist, explains that chronic activation of this stress response system literally shrinks the hippocampus—the brain region responsible for memory and learning—while enlarging the amygdala, making you more reactive to future stressors. MRI studies show that people with chronic stress have measurably smaller brain volume in areas crucial for decision-making and emotional regulation.
Stress Effects on the Body: Gut and Digestive System Explained
The hormonal chaos doesn’t stop there. Elevated cortisol disrupts your body’s natural circadian rhythms, suppressing melatonin production and fragmenting sleep. This creates a vicious cycle: poor sleep increases stress hormones, which further impair sleep quality. Meanwhile, chronically high cortisol levels interfere with insulin sensitivity, often leading to weight gain around the midsection and increased risk of type 2 diabetes.
How stress affects the body becomes particularly evident in the brain’s reward pathways. Chronic stress actually rewires neural circuits, making you crave high-fat, high-sugar foods while simultaneously reducing your ability to experience pleasure from healthy activities. This neurological hijacking explains why stressed individuals often turn to comfort food, alcohol, or other substances for relief.
Chronic Stress & Your Immune System Breakdown
Your immune system and stress response system are intimately connected through a complex network of chemical messengers called cytokines. Under normal circumstances, short-term stress actually boosts immunity, mobilizing white blood cells to fight potential infections or heal injuries.
But chronic stress flips this protective response on its head.
Research published in Psychological Science reveals that people under chronic stress produce significantly fewer antibodies in response to vaccines, leaving them vulnerable to infections they would normally fight off easily. The mechanism is both elegant and devastating: persistent cortisol elevation suppresses the production of lymphocytes (T-cells and B-cells), the immune system’s specialized warriors against pathogens and cancer cells.
Stress Effects on the Body: Impact on Heart and Cardiovascular Health
Dr. Janice Kiecolt-Glaser’s groundbreaking studies at Ohio State University show that caregivers of Alzheimer’s patients—individuals under extreme chronic stress—take up to 40% longer to heal from wounds compared to age-matched controls. Their immune systems are so compromised that even minor cuts become prolonged healing challenges.
The cellular damage goes deeper. Chronic stress accelerates the shortening of telomeres, the protective caps on chromosomes that determine cellular aging. Nobel Prize-winning research by Elizabeth Blackburn demonstrates that women caring for chronically ill children had telomeres equivalent to someone a decade older, literally aging them at the genetic level.
Perhaps most concerning is stress’s impact on cancer surveillance. Natural killer (NK) cells patrol your body 24/7, identifying and destroying abnormal cells before they become tumors. Chronic stress significantly reduces NK cell activity, potentially explaining why stressed individuals show higher rates of cancer recurrence and progression.

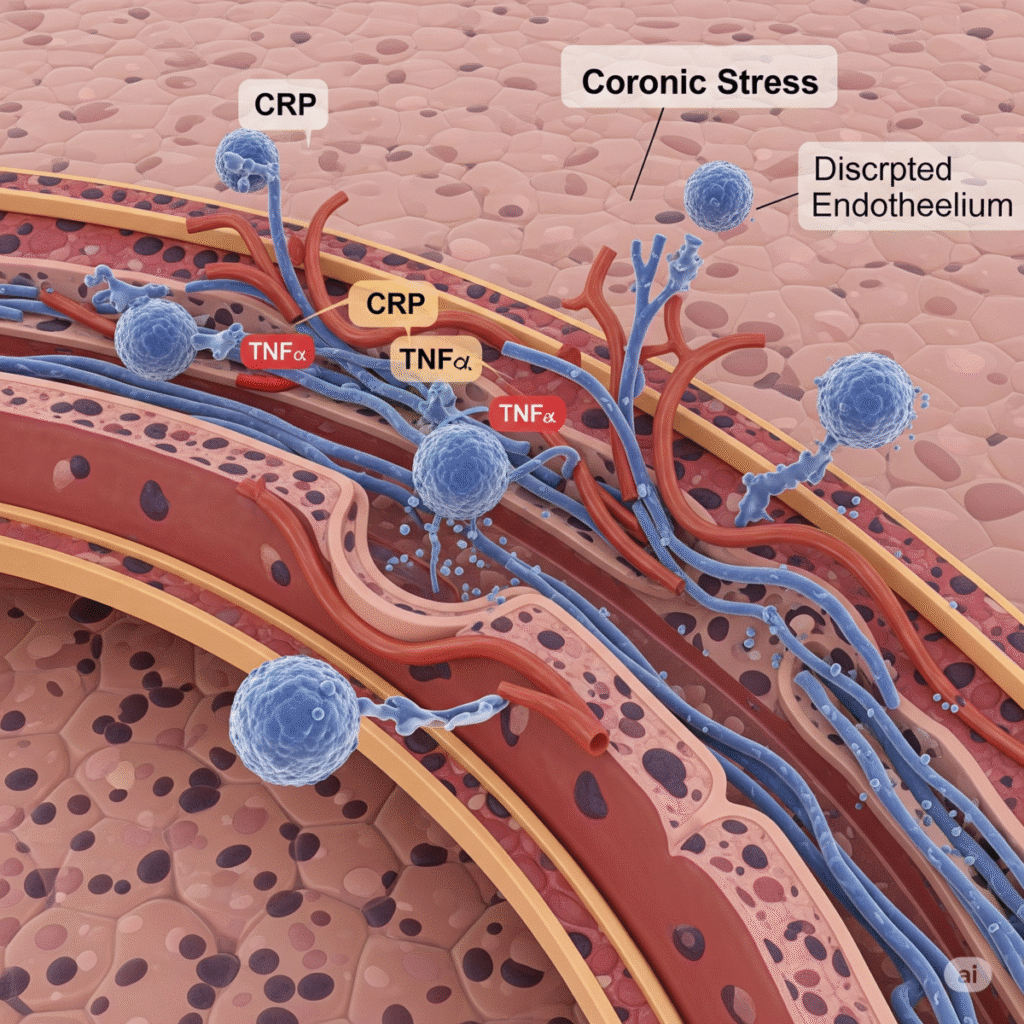
Stress and Inflammation: The Silent Killers
Inflammation is your body’s natural healing response to injury or infection. But when stress becomes chronic, it triggers a state of systemic inflammation that never fully resolves—like having a fire that never gets completely extinguished, just keeps smoldering.
The key player in this inflammatory cascade is a protein complex called NF-κB (nuclear factor kappa B). Chronic stress keeps NF-κB constantly activated, leading to the overproduction of inflammatory molecules like interleukin-6, tumor necrosis factor-alpha, and C-reactive protein. These inflammatory markers don’t just indicate disease—they actively promote it.
Dr. Steve Cole’s research at UCLA reveals that people under chronic stress show a “conserved transcriptional response to adversity” (CTRA)—essentially, their genes get stuck in an inflammatory pattern that persists even after the stressor is removed. This genetic expression pattern is linked to accelerated aging and increased risk of heart disease, diabetes, arthritis, and neurodegenerative diseases.
Stress Effects on the Body: How the Brain Reacts to Anxiety
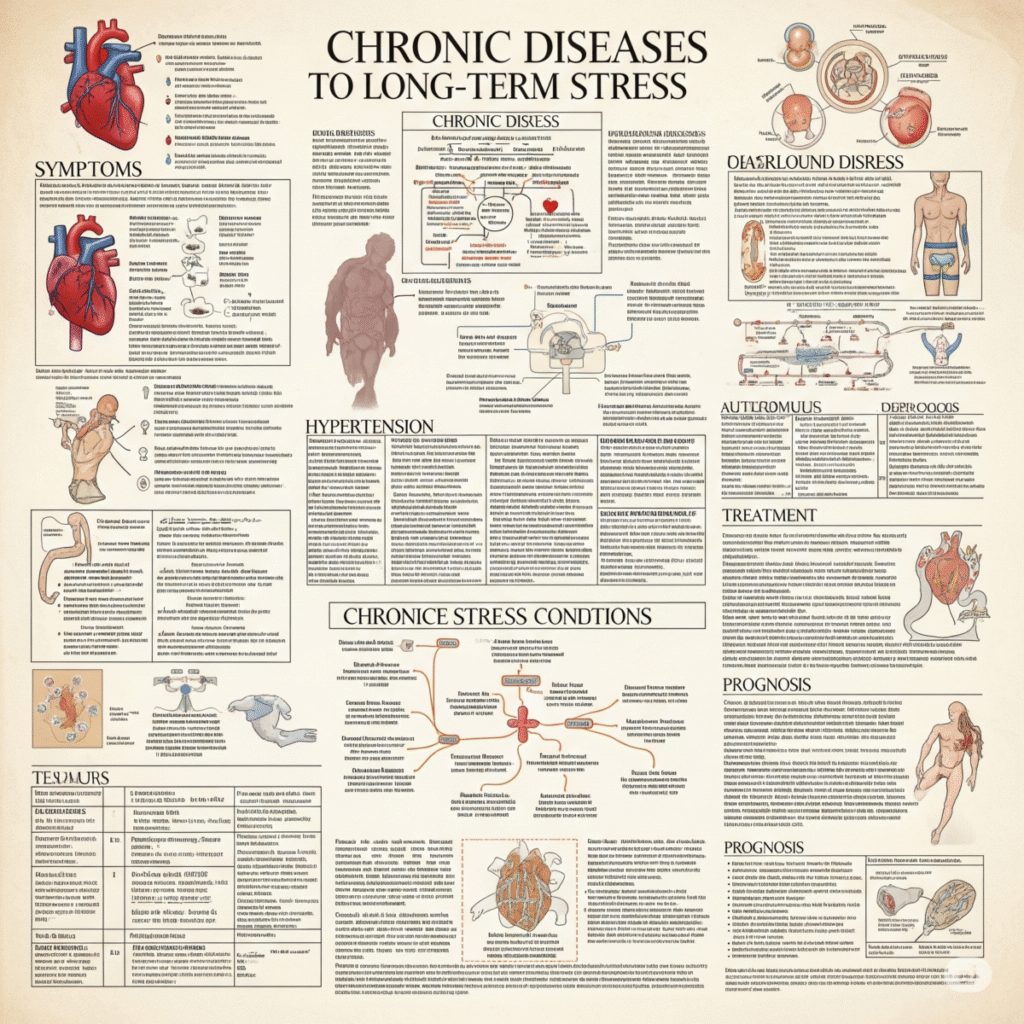
The inflammatory effects of chronic stress are particularly visible in conditions like:
- Autoimmune disorders: Stress-induced inflammation can trigger the immune system to attack healthy tissue, leading to conditions like rheumatoid arthritis, lupus, and multiple sclerosis.
- Skin conditions: Chronic stress exacerbates inflammatory skin conditions like eczema, psoriasis, and acne by increasing inflammatory cytokines and disrupting the skin’s barrier function.
- Digestive issues: Inflammation in the gut lining can lead to increased intestinal permeability (“leaky gut”), inflammatory bowel disease, and irritable bowel syndrome.
The connection between stress and inflammation helps explain why how stress affects the body extends far beyond temporary discomfort—it creates the biological foundation for multiple chronic diseases to take root simultaneously.
Is Your Heart at Risk? Stress and Cardiovascular Impact
Your cardiovascular system bears the brunt of chronic stress in ways that can be immediately life-threatening. The American Heart Association now recognizes chronic stress as a major risk factor for heart disease, on par with smoking, high blood pressure, and high cholesterol.
When stress hormones surge, they don’t just make your heart beat faster—they fundamentally alter how your cardiovascular system functions. Adrenaline and cortisol cause blood vessels to constrict, forcing your heart to pump harder against increased resistance. Over time, this leads to hypertension, even in people with previously normal blood pressure.
The Whitehall Studies, following British civil servants for decades, revealed that work-related stress increases heart disease risk by 68%. The mechanism involves multiple pathways: chronic stress promotes the formation of atherosclerotic plaques, makes existing plaques more likely to rupture, and increases blood clotting factors that can trigger heart attacks and strokes.
Dr. Redford Williams at Duke University discovered that people with high hostility and time urgency—classic markers of chronic stress—show exaggerated cardiovascular responses to daily challenges. Their blood pressure spikes higher and stays elevated longer than resilient individuals, creating a constant state of cardiovascular strain.
The heart-stress connection becomes particularly dangerous during acute stress events. Studies show that heart attacks increase significantly following natural disasters, terrorist attacks, and even sports events that trigger intense emotional responses. The “broken heart syndrome” (takotsubo cardiomyopathy) literally demonstrates how extreme emotional stress can cause heart muscle dysfunction identical to a heart attack.
How stress affects the body’s cardiovascular system also includes changes in heart rate variability—the healthy variation between heartbeats that indicates a resilient nervous system. Chronic stress reduces heart rate variability, a marker associated with increased risk of sudden cardiac death and overall mortality.

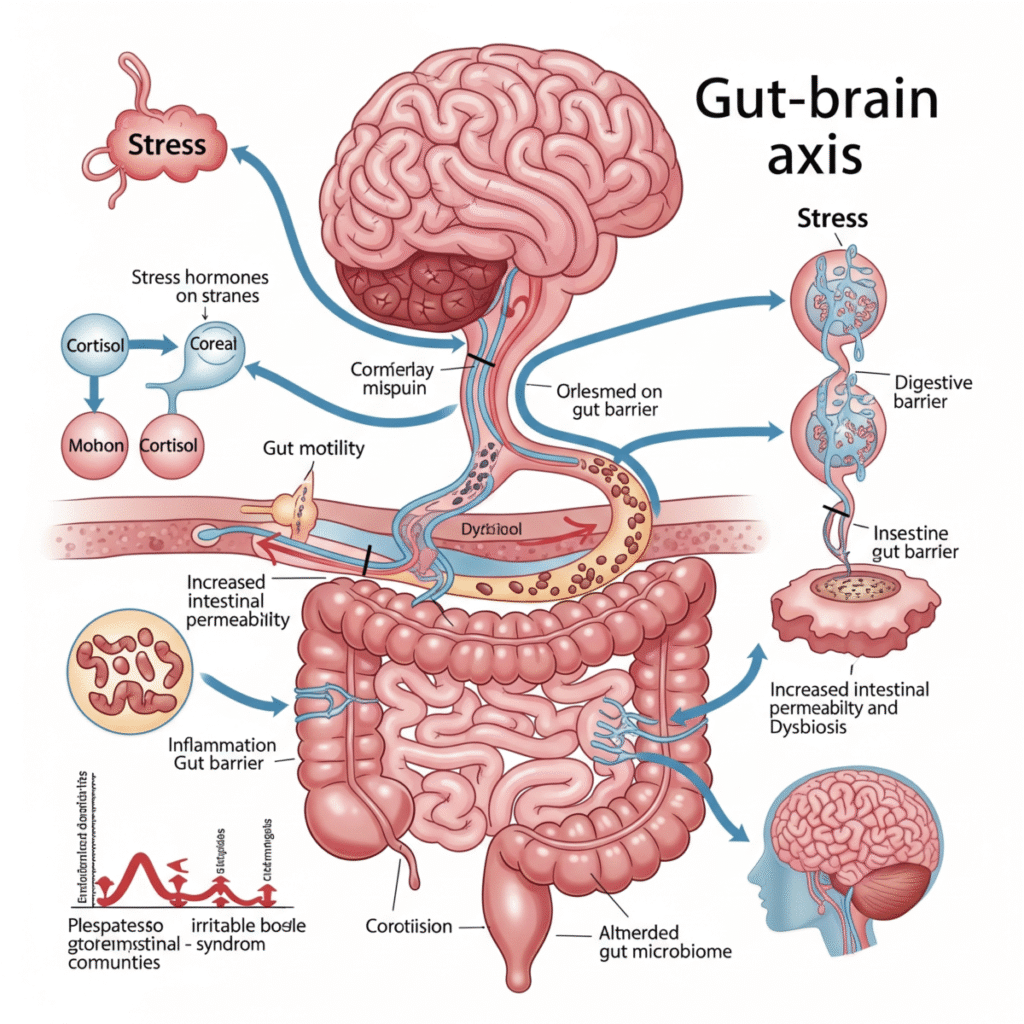
Stress and the Gut-Brain Axis: The Mind in Your Belly
Scientists are discovering that your gut is essentially a “second brain,” containing over 500 million neurons and producing 95% of your body’s serotonin. This gut-brain axis represents a bidirectional communication superhighway where stress in your mind directly impacts your digestive system, and gut dysfunction can worsen stress and anxiety.
When you experience chronic stress, it literally changes the composition of your gut microbiome—the trillions of bacteria that help digest food, produce vitamins, and regulate immune function. Research from UCLA shows that stressed individuals have significantly less microbial diversity and fewer beneficial bacteria like lactobacillus and bifidobacterium.American Psychological Association (APA) – Stress Effects on the Body
This bacterial imbalance has profound effects on both physical and mental health. Beneficial gut bacteria produce short-chain fatty acids that reduce inflammation and support brain health. When stress depletes these protective microbes, it creates a cascade of problems: increased intestinal permeability (leaky gut), heightened inflammatory responses, and altered neurotransmitter production.
Dr. Emeran Mayer’s groundbreaking research at UCLA demonstrates that gut bacteria actually influence brain function through the vagus nerve, the longest cranial nerve connecting your brain to your digestive system. When chronic stress disrupts the gut microbiome, it can contribute to anxiety, depression, and cognitive fog—creating a vicious cycle where gut dysfunction worsens stress, which further damages gut health.
The physical symptoms are equally concerning. Chronic stress can trigger or exacerbate:
- Irritable bowel syndrome (IBS)
- Inflammatory bowel disease
- Gastroesophageal reflux disease (GERD)
- Peptic ulcers (especially when combined with H. pylori bacteria)
- Food sensitivities and allergies
Understanding how stress affects the body through the gut-brain axis has revolutionized treatment approaches, with many physicians now recommending probiotics, fermented foods, and stress reduction techniques as integrated therapies for both digestive and mental health conditions.
The Long-Term Toll: Diseases Triggered by Prolonged Stress
The cumulative impact of chronic stress on the body creates what researchers call “allostatic load”—the physiological cost of constantly adapting to stress. Over time, this load becomes so heavy that multiple body systems begin to break down simultaneously, often manifesting as seemingly unrelated chronic diseases.
Large-scale epidemiological studies reveal that people with high chronic stress have significantly increased risks of:
Metabolic Disorders: Chronic cortisol elevation promotes insulin resistance, leading to type 2 diabetes, metabolic syndrome, and obesity. The Nurses’ Health Study found that women with the highest stress levels were 17% more likely to develop diabetes, independent of other risk factors.
Neurodegenerative Diseases: Chronic inflammation and elevated cortisol levels accelerate brain aging and increase the risk of Alzheimer’s disease and dementia. The stress hormone cortisol is particularly toxic to hippocampal neurons involved in memory formation.
Cancer: While stress doesn’t directly cause cancer, it creates conditions that promote cancer development and progression. Chronic stress suppresses immune surveillance, promotes angiogenesis (blood vessel formation that feeds tumors), and increases metastatic potential through inflammatory pathways.
Autoimmune Conditions: The dysregulated immune response caused by chronic stress can trigger the development of autoimmune diseases like rheumatoid arthritis, lupus, and multiple sclerosis. Stress doesn’t just worsen these conditions—it may be a primary trigger in genetically susceptible individuals.
Accelerated Aging: At the cellular level, chronic stress accelerates biological aging through multiple mechanisms: telomere shortening, increased oxidative stress, mitochondrial dysfunction, and chronic inflammation. This explains why people under severe chronic stress often look and feel years older than their chronological age.
The interconnected nature of these stress-related diseases means that having one condition significantly increases the risk of developing others—creating a cascade of declining health that can be difficult to reverse once established.
Reversing the Damage: Mindfulness, Sleep, and Recovery
The remarkable news is that many of the harmful effects of chronic stress can be reversed through evidence-based interventions that address both the psychological and physiological aspects of the stress response.
Mindfulness and Meditation: Research by Dr. Sara Lazar at Massachusetts General Hospital shows that just eight weeks of mindfulness meditation can increase gray matter in the hippocampus (the brain region damaged by chronic stress) while shrinking the amygdala (the brain’s alarm center). These structural brain changes correspond with improved stress resilience and emotional regulation.
Mindfulness practices work by activating the parasympathetic nervous system—your body’s “rest and digest” mode—which directly counteracts the stress response. Studies show that regular meditation practitioners have lower cortisol levels, reduced inflammatory markers, and stronger immune function compared to non-practitioners.
Sleep Restoration: Quality sleep is perhaps the most powerful antidote to chronic stress. During deep sleep, your brain literally cleanses itself of toxic proteins that accumulate during waking hours, including amyloid beta associated with Alzheimer’s disease. Sleep also allows cortisol levels to naturally reset to their healthy circadian rhythm.
Creating optimal sleep conditions involves more than just duration—it requires consistent sleep and wake times, a cool, dark environment, and limiting screen exposure before bedtime. Research shows that improving sleep quality can reduce inflammatory markers within weeks and begin restoring healthy immune function.
Physical Exercise: Regular exercise acts as a form of “stress inoculation,” teaching your body to efficiently activate and then recover from the stress response. Aerobic exercise increases production of brain-derived neurotrophic factor (BDNF), which promotes the growth of new neurons and helps repair stress-related brain damage.
The key is finding the right exercise intensity. While moderate exercise reduces stress and inflammation, excessive high-intensity training can actually increase cortisol levels and worsen stress-related symptoms.
Social Connection: Strong social relationships are among the most powerful predictors of stress resilience and longevity. The Harvard Study of Adult Development, spanning over 80 years, consistently shows that people with strong social ties have lower cortisol levels, better immune function, and significantly reduced risk of chronic disease.
Understanding how stress affects the body empowers you to take targeted action to interrupt these destructive processes before they become irreversible.

Physical signs that stress is impacting your body include fatigue, headaches, muscle tension, digestive issues, and sleep problems. Emotionally, you may feel anxious, irritable, or overwhelmed. If these signs persist, stress could be silently damaging your health.
Yes. Chronic stress weakens your immune system and increases inflammation, contributing to conditions like heart disease, diabetes, and gut disorders. The mind-body connection means emotional stress can manifest as physical illness.
Healing time varies, but with regular stress-reduction practices, improvements in sleep and mood may appear in 2-4 weeks. Deeper healing of inflammation and brain changes may take 6-12 weeks or longer.
Stress affects gut health by disrupting the microbiome, increasing gut permeability, and triggering IBS or acid reflux. This gut-brain connection plays a major role in how your body responds to stress.
Many effects of chronic stress are reversible with lifestyle changes like meditation, better sleep, and therapy. However, some damage to the heart or brain may need medical help in addition to personal healing practices.
Stress raises cortisol, which promotes belly fat and sugar cravings. It also disturbs appetite-regulating hormones, leading to emotional eating and poor sleep—factors that cause and maintain weight gain.
Acute stress is short-term and can improve performance. Chronic stress is long-lasting and damages body systems by keeping cortisol levels high. The key is allowing your body time to recover and heal from stressors.
Your Body Is Listening—Start Healing Today
The science is clear: how stress affects the body extends far beyond temporary discomfort. Chronic stress creates a cascade of biological changes that age you prematurely, weaken your defenses against disease, and rob you of the vitality you deserve. But within this sobering reality lies tremendous hope—your body possesses remarkable healing capabilities when given the right conditions to recover.
Every moment of mindfulness, every quality night of sleep, every gentle movement, and every meaningful connection with others sends powerful healing signals throughout your system. Your immune cells become more vigilant, your brain begins to repair itself, and your cardiovascular system starts to find its natural rhythm again.
The transformation doesn’t require perfection—it requires consistency. Start with one evidence-based practice today: try five minutes of deep breathing, prioritize seven hours of sleep tonight, or reach out to someone you care about. Your body has been faithfully carrying the burden of your stress; now it’s time to give it the support it needs to heal.
Your body hears everything your mind says. Start healing now.
For more evidence-based strategies to reclaim your health, explore our comprehensive guide: Best Natural Anxiety Relief Techniques in 2025





Leave a Reply